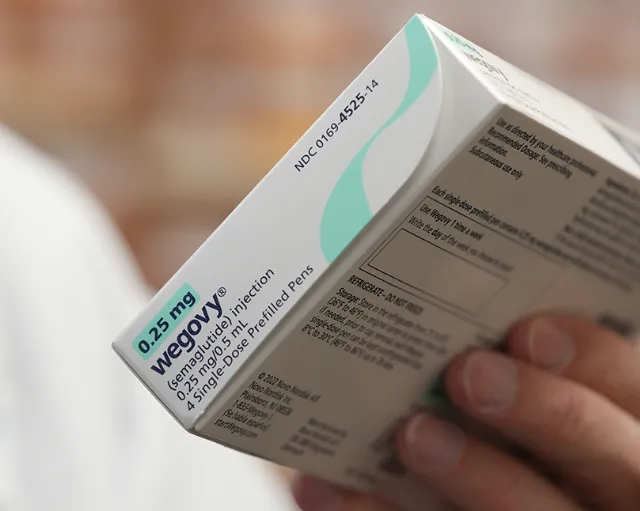
Medications such as Ozempic, Wegovy, Mounjaro, and Zepbound have transformed the conversation around obesity and related health concerns. Known as GLP-1 receptor agonists, these drugs have been shown to help with significant weight reduction and improved metabolic health. The challenge? Their steep price tag—often topping $1,000 per month without insurance—has many patients asking whether their health plan will help cover the cost.
The short answer is: it depends. Insurance coverage varies widely depending on the type of plan you have, how the medication is prescribed, and the rules in your state.
Insurance and GLP-1 Coverage
Employer and Private Insurance
Some workplace and ACA marketplace health plans cover GLP-1 drugs when prescribed for obesity treatment, while others exclude them as “lifestyle” medications. Coverage tends to be more reliable when these drugs are prescribed for Type 2 diabetes, since insurers classify that as a medical necessity.
Medicare and Medicaid
- Medicare: By law, Medicare Part D does not cover drugs prescribed solely for weight loss. However, medications like Ozempic may be covered when prescribed for diabetes.
- Medicaid: Coverage differs by state. A few states approve GLP-1s for weight management, but many limit coverage to diabetes treatment only.
Why Coverage Is Often Restricted
Insurers have been hesitant to fully embrace weight-loss medications for a few reasons:
- High price tags: Out-of-pocket costs are typically over $1,000 per month.
- Long-term treatment concerns: Many patients need to stay on the medication to maintain results, raising overall costs.
- Classification disputes: Some insurers still categorize obesity drugs as non-essential, despite growing medical recognition of obesity as a serious condition.
Common Questions
If my doctor prescribes a GLP-1, will my insurance automatically cover it?
Not necessarily. Even with a prescription, your insurance may deny coverage if the drug isn’t listed on your plan’s formulary.
Do insurers usually require prior authorization?
Yes. Approval often requires proof of a certain BMI, related health conditions such as hypertension or diabetes, and documentation of unsuccessful lifestyle-based weight loss attempts.
Can I appeal if my claim is denied?
Yes. Patients have the right to appeal denials, and providing medical documentation can improve the chances of approval.
Steps to Improve Your Chances of Coverage
- Check your plan’s formulary to see if Ozempic, Wegovy, Mounjaro, or Zepbound are included.
- Work with your doctor to provide medical records or a letter of necessity.
- Submit prior authorization requests with details on BMI, comorbidities, and past weight-loss efforts.
- File an appeal if your claim is denied—ACA rules give you the right to internal and external reviews.
- Look into patient assistance programs or manufacturer savings cards, which can help lower out-of-pocket costs.
Bottom Line
GLP-1 drugs represent an important new option for weight management, but insurance coverage is still inconsistent. Most health plans are more likely to cover them for diabetes than for obesity alone. If you’re considering one of these medications, the best approach is to review your plan’s formulary carefully, work with your healthcare provider to prepare supporting documentation, and use the appeals process if coverage is denied.
For many patients, persistence and documentation can make the difference between paying full price and getting the support needed to access these treatments.